Introduction and plan overview
The 2024-2029 Arizona Cancer Control Plan (AzCCP) is the state’s five-year strategy to fight against cancer and reduce the cancer burden. It serves as a collaboration among individuals and organizations committed to improving Arizona’s cancer incidence and mortality rates. It has been said, “Cancer affects everyone, but not everyone equally.” With that said, this plan focuses on addressing the disproportionate systematic, environmental and socio-economic impact cancer has on Arizona’s residents in specific geographic areas most affected by cancer and cancer risk factors.
In its fourth edition, the 2024-2029 AzCCP is a living instrument that aims to implement evidence-based strategies to reduce the burden of cancer across the cancer care continuum for all Arizonans.
Through community listening sessions, workgroup meetings, and input from experts in the community the AzCCP was developed to continue to build upon the work of the 2020-2024 cancer plan, and also explore cancer related issues that have emerged in the last five years. In collaboration with a diverse group of stakeholders including, providers, community organizations, and individuals who have been affected by cancer, the coalition was able to build a plan that reflects the most timely cancer topics in the state, implements the most recent evidence based strategies, and address the barriers that Arizonans face when accessing education, resources, care, and support.
According to the National Cancer Institute, the cancer control continuum is used to describe the various stages from cancer etiology, prevention, early detection, diagnosis, treatment, survivorship, and end of life.It is a useful framework on which to view plans, progress, and priorities. It helps us identify research gaps, where we must collaborate with others to have an impact, and where more resources may be needed. The objectives in the cancer plan span the entire continuum with the goal of helping as many people as possible regardless of where they are in their cancer journey.

It is our hope that after reading the AzCCP, you feel you have gained the knowledge, tools, and resources needed to be informed and empowered cancer advocates.
Development process
The five-year AzCCP was developed by members of the Arizona Cancer Coalition (AzCC). Coalition members are individuals, community members, professionals, and the cancer survivors who share their expertise, resources, and ideas. They are committed to improving cancer control priorities and reducing disparities in hopes of a cancer-free Arizona. The coalition is open to anyone who is passionate about reducing the cancer burden in Arizona.
The AzCC and the Arizona Comprehensive Cancer Cancer Control Program (AzCCCP) held a series of listening sessions to collect feedback on priority areas and engage with community members. Through these listening sessions topic areas were identified and categorized based on which of the five workgroups within the coalition structure were the most appropriate.
These five workgroups include: Early Detection and Prevention, Survivorship and Quality of Life, Treatment, Policy, and Childhood Cancer. Once the topic areas were identified smaller teams convened to identify the objectives, within each of the workgroups. These objectives were then reviewed by coalition and community leaders to make sure that they addressed the guiding principles established by the coalition leadership team.
These guiding principles included a focus on health equity, including diverse stakeholders, alignment with existing programing, ensuring the plan was data driven and measurable, and that the process for developing the plan was transparent. After implementing feedback from the reviewers, the teams met again to identify the strategies to be implemented over the next five years to accomplish the objectives.
At the end of the process individuals from more than 50 organizations participated in the drafting, editing, and approval of the new cancer plan. Over the next five years the workgroups will be responsible for developing, implementing, and evaluating the Program. They will work collectively to achieve the plan's goals and to make a positive, lasting impact on the Arizona cancer community.
Dedication
This plan is dedicated to those whose lives have been touched by cancer. Whether a patient, provider, family member, or survivor, let this plan serve as a tool and tribute to your incredible spirit.
Cancer data
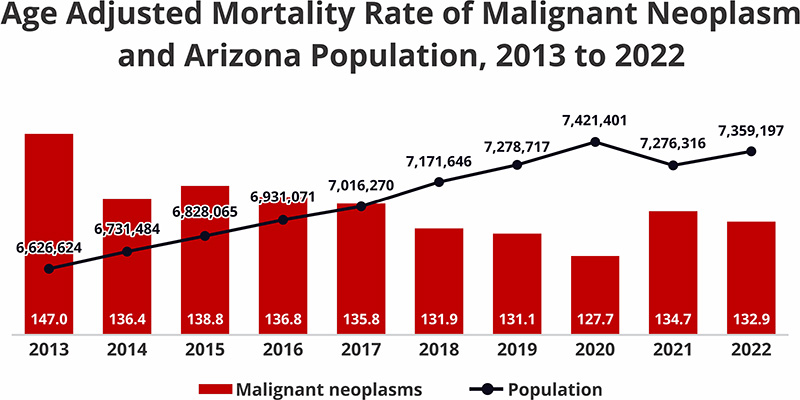
Between 2013 and 2022 malignant neoplasm has remained a burden in Arizona. The mortality rate (per 100,000) of malignant neoplasm only decreased by 10% over the past 10 years, whereas the population of Arizona increased by 10% over the same time period.
In 2022, malignant neoplasm was ranked the second leading cause of death in Arizona with 13,171 deaths in the state(132.0 per 100,000).
Top 10 Leading Causes of Death in Arizona, 2022
| Leading causes of death | Deaths | Age-adjusted rate | Rank |
| Diseases of heart | 14,593 | 148.5 | 1 |
| Malignant neoplasms (Cancer) | 13,171 | 132.9 | 2 |
| Accidents (unintentional injuries) | 5,929 | 75.6 | 3 |
| COVID-19 | 4,608 | 47.4 | 4 |
| Chronic lower respiratory diseases | 3,577 | 35.1 | 5 |
| Cerebrovascular diseases | 3,390 | 34.5 | 6 |
| Alzheimer disease | 2,823 | 28.4 | 7 |
| Diabetes mellitus | 2,424 | 25.1 | 8 |
| Intentional self-harm (suicide) | 1,604 | 20.6 | 9 |
| Chronic liver disease and cirrhosis | 1,492 | 17.5 | 10 |
The Arizona Cancer Registry (ACR) is a program that collects, manages and analyzes information on the incidence and survival of Arizona residents diagnosed with cancer. The registry receives cancer cases from hospitals, free-standing clinics, physician offices, pathology laboratories, data exchanges and death certificates.
The data that the registry collects is used to represent Arizona’s cancer burden. To measure the cancer burden, cancer registries utilize age-adjusted rates. Age-adjusted rates show the number of cases or deaths occurring in every 100,00 people within a specific population and time frame. “Rate”= Age-Adjusted Rate.
The impact of the COVID-19 Pandemic on patients with cancers and cancer data reporting is reflected in the data available for 2020 and 2021. Fluctuations in cancer incidence and mortality rates may be due to delays in diagnosis, lack of screening, disruption of patient treatment and follow-up care and unforeseen health complications due to contracting COVID-19.
Arizona cancer incidence, 2017 to 2021
Cancer incidence refers to new cancer cases diagnosed in Arizona.
Table 1.1: Aggregate Case Counts and Age-Adjusted Incidence Rates for Invasive Cancer in Arizona, 2017 to 2021
| Diagnosis years | Case counts | Age-adjusted rates |
| 2017-2021 | 175,500 | 394.5 |
Between 2017 and 2021, a total of 175,000 Arizonans were diagnosed with invasive cancer at a rate of 394.5 cases per 100,000 Arizonans. Arizona invasive cancer diagnoses have decreased 7% from 2017 to 2021.
Table 1.2: Aggregate Case Counts and Age-Adjusted Incidence Rates for Invasive Arizona Cancer Cases by Race/Ethnicity, 2017 to 2021
| Race/Ethnicity | Case counts | Age-adjusted rates |
| White Non-Hispanic | 138,054 | 431.6 |
| White Hispanic | 20,863 | 284.3 |
| Black/African American | 5,551 | 342.9 |
| American Indian/Alaskan Native | 4,060 | 263.8 |
| Asian/Pacific Islander | 3,226 | 227.5 |
| Unknown Race | 3,746 | N/A |
In Arizona, White Non-Hispanic individuals have the highest cancer incidence rate (431.6 cases per 100,000 people). Asian and Pacific Islanders in Arizona have the lowest cancer incidence rate (227.5 cases per 100,000 people).
Table 1.3: Aggregate Case Counts and Age-Adjusted Incidence Rate for Invasive Arizona Cancer Cases by Sex, 2017 to 2021
| Sex | Case counts | Age-adjusted rates |
| Males | 90,018 | 418.3 |
| Females | 85,482 | 378.9 |
Arizona males have higher rates of invasive cancer compared to Arizona females. Males have a 10% higher rate of invasive cancer diagnoses compared to females.
Table 1.4: Aggregate Case Counts and Age-Adjusted Incidence Rates for Top Five Invasive Cancer Sites in Arizona, 2017 to 2021
| Cancer site | Case counts | Age-adjusted rates |
| Female Breast | 26,298 | 118.7 |
| Lung and Bronchus | 20,176 | 42.6 |
| Prostate | 18,489 | 80.7 |
| Melanoma | 13,946 | 31.7 |
| Colorectal | 13,946 | 32.0 |
The most common cancer types among Arizonans: female breast, lung and bronchus, prostate, colorectal cancer and melanoma. Arizona’s melanoma rate is higher than the national melanoma rate (23.0 cases per 100,000 people).
Table 1.5: Percentage of Arizona Cancer Cases by Stage at Diagnosis* for Selected Cancer Sites, 2017 to 2021
| Female breast | Lung and bronchus | Prostate | Melanoma | Colorectal | Cervical** | |
| Early stage | 71.3% | 26.9% | 66.0% | 93.1% | 31.2% | 43.0% |
| Late stage | 24.7% | 59.9% | 23.5% | 5.0% | 58.3% | 43.2% |
| Unknown stage | 4.0% | 13.2% | 10.5% | 1.5% | 10.5% | 13.7% |
*Early Stage = In situ and Local Stage using SEER Summary Stage.
Late Stage = Regional and Distant Stage using SEER Summary Stage.
Unknown Stage = Stage at diagnosis not documented.
**Cervical cancer Early Stage includes Local Stage only; In situ cases are excluded from this data.
Lung and bronchus and colorectal cancer are being diagnosed at later stages and cervical cancer is being diagnosed equally at early and later stages (in situ cervical cases not included). These cancers are being diagnosed in later stages despite available lung, colorectal and cervical cancer screening, and vaccinations available to prevent potential cervical cancer cases.
Median Age at Diagnosis = 68 years old
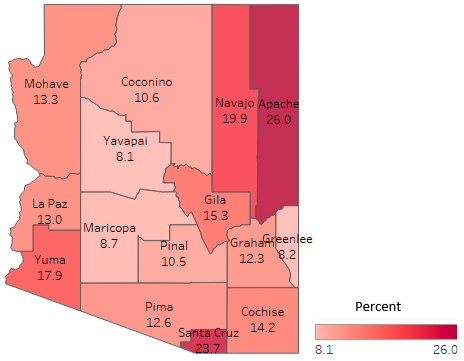
Figure 1.1: Aggregate Age-Adjusted Incidence Rates for Invasive Cancer Cases by County in Arizona, 2017 to 2021
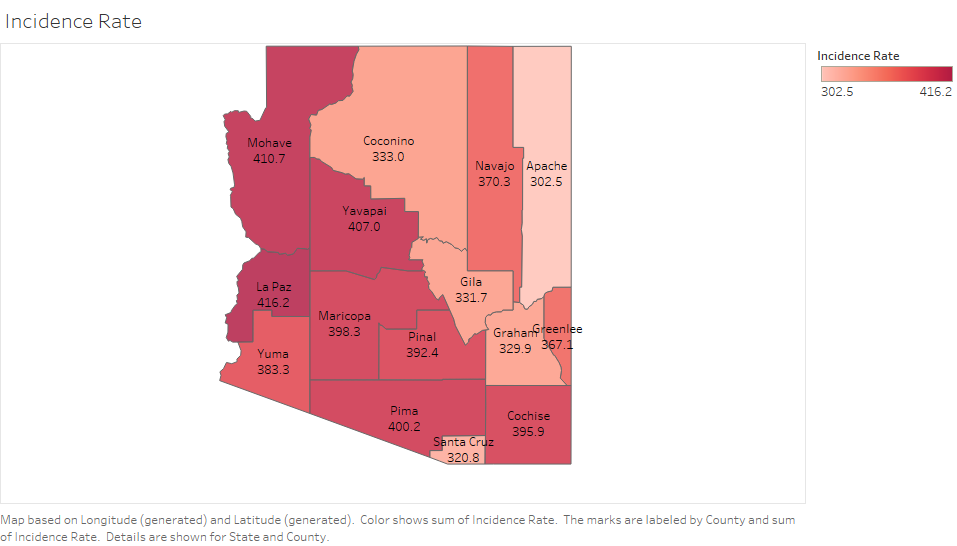
Between 2017 and 2021, Mohave and La Paz Counties have the highest cancer incidence rates while Apache and Santa Cruz Counties have the lowest cancer incidence rate in Arizona.
Arizona cancer mortality data, 2018 to 2022
Cancer mortality refers to cancer deaths occurring in Arizona.
Table 2.1: Aggregate Number of Deaths and Age-Adjusted Mortality Rates (per 100,000 people) for Cancer Deaths in Arizona, 2018 to 2022
| Year of death | Number of deaths | Age-adjusted rates |
| 2018-2022 | 63,193 | 134.1 |
Between 2018 and 2022, a total of 63,193 Arizonans died of cancer at a rate of 134.1 deaths per 100,000 Arizonans. Arizona cancer deaths have decreased 4% from 2018 to 2022.
Table 2.2: Aggregate Number of Deaths and Age-Adjusted Mortality Rates (per 100,000 people) for Arizona Cancer Deaths by Race/Ethnicity, 2018 to 2022
| Race/Ethnicity | Number of deaths | Age-adjusted rates |
| White Non-Hispanic | 49,531 | 138.1 |
| White Hispanic | 8,306 | 121.8 |
| Black/African American | 2,268 | 149.1 |
| American Indian/Alaskan Native | 1,548 | 108.4 |
| Asian/Pacific Islander | 1,227 | 89.3 |
| Unknown Race | 313 | N/A |
In Arizona, Black/African American individuals have the highest cancer mortality rates (149.1 deaths per 100,000 people). Asian and Pacific Islanders in Arizona have the lowest cancer mortality rates (89.3 deaths per 100,000 people).
Table 2.3: Aggregate Number of Deaths and Age-Adjusted Mortality Rates of Arizona Cancer Cases by Sex, 2018 to 2022
| Sex | Number of deaths | Age-adjusted rates |
| Males | 34,023 | 155.3 |
| Females | 29,170 | 116.9 |
Arizona males have higher rates of cancer deaths compared to Arizona females. Males have a 25% higher rate of cancer deaths compared to females.
Table 2.4: Aggregate Number of Deaths and Age-Adjusted Mortality Rates (per 100,000) for Top 5 Cancer Sites in Arizona, 2018 to 2022
| Cancer site | Number of deaths | Age-adjusted rates |
| Lung and bronchus | 12,813 | 26.3 |
| Colorectal | 5,644 | 12.3 |
| Pancreas | 5,019 | 10.4 |
| Female Breast | 4,509 | 18.8 |
| Prostate | 3,758 | 17.6 |
The cancer types responsible for the most cancer related deaths in Arizona: lung and bronchus, colorectal, pancreatic, female breast and prostate.
Median Age at Death = 73 years old
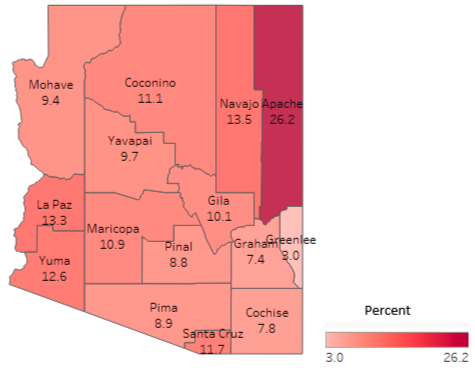
Figure 2.1: Aggregate Age-Adjusted Mortality Rates for Cancer Deaths by County in Arizona, 2018 to 2022
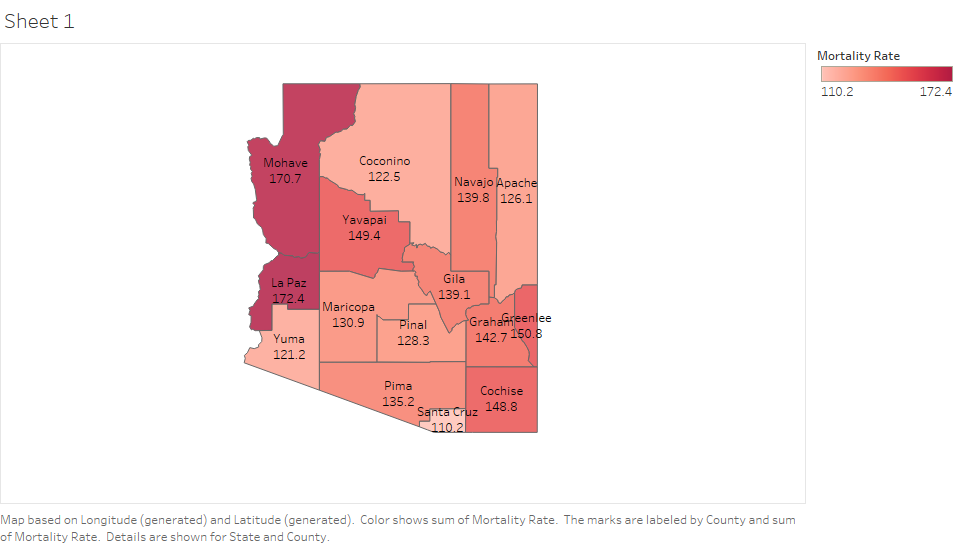
Between 2018 and 2022, Mohave and La Paz Counties have the highest cancer mortality rates while Santa Cruz and Yuma Counties have the lowest cancer mortality rate in Arizona.
Data cited in the plan includes information from the Arizona Cancer Registry, Centers for Disease Control, and the Arizona Social Vulnerability Index.
The Arizona Cancer Coalition
The Arizona Cancer Coalition (AzCC) is a diverse group of clinical, community, and civic stakeholders who are passionate about reducing Arizona’s cancer burden.
The AzCC is composed of five primary work groups each focusing on a different area of the cancer care continuum. These work groups mirror the priority areas in the cancer plan and include Early Detection and Prevention, Treatment, Survivorship and Quality of Life, Policy, and Childhood Cancer. These work groups are responsible for developing, implementing, and evaluating the comprehensive cancer control plan and work collectively to achieve the plan's goals and to make a positive, lasting impact on the Arizona cancer community.
Vision: To secure a future where cancer prevention, early detection, treatment, and survivorship are accessible and equitable for all Arizonans. Through collaborative partnerships, innovative approaches, and advocacy, we aim to create a culture of health that prioritizes cancer prevention, supports those affected by cancer, and fosters a statewide commitment to eradicating this disease. Together, we strive towards a brighter tomorrow where cancer is no longer a threat to the well-being and vitality of our communities.
Mission: To reduce the burden of cancer through collaborative efforts in prevention, early detection, treatment, policy, and survivorship.
To make the plan easier to navigate, The Arizona Comprehensive Cancer Control Program (AzCCCP) will be referred to as the “Program”. The Arizona Cancer Coalition (AzCC) will be referred to as the “Coalition” and the Arizona Cancer Control Plan (AzCCP), will be referred to as the “Plan”.
Early detection and prevention
The easiest way to fight cancer is to stop it before it starts. Many cancers are preventable. Primary prevention helps people choose healthy behaviors to lower their risk of getting cancer. Preventative screenings help identify lesions before they can turn cancerous.
Completing recommended cancer screenings in a timely manner are vital for early detection and effective treatment, greatly improving health outcomes.Timely screenings help find these diseases at an early stage, when treatment works best. Early detection and prevention are among the most effective tools in the fight against cancer.
Aside from their practicality and cost-effectiveness, the benefits of early detection and prevention can be seen at the individual, community and societal levels.
By June of 2029
Objective one: Decrease the percentage of late stage prostate cancer diagnosis from 25% to 23%.
Strategies
- Increase public awareness by exploring and developing mass media options employing print and electronic media for public service prostate cancer awareness announcements.
- Perform Community outreach by partnering with (a) community-based organizations to promote prostate cancer awareness and screenings among diverse populations with elevated prostate cancer incidence/mortality risk, and (b) businesses/their insurers to promote prostate cancer awareness/education/screenings and participating in at least two community based events, at least one of which is geographically remote, annually to promote prostate cancer awareness and screenings among diverse populations with elevated prostate cancer incidence/mortality risk.
- Explore the process in collaboration with the Policy Screening work group for State funding (license plate) to be allocated to prostate cancer awareness/screening programs (similar to WellWoman HealthCheck Program). Implement based on findings.
Prostate cancer cost data
$81,483 - The average cost of prostate cancer related hospital discharges in Arizona in 2022.
Approximately $55 million in total charges were spent on prostate cancer related hospital discharges in Arizona in 2022.
Prostate cancer is the most common cancer diagnosis for Arizona males. Black/African American males had the highest age-adjusted incidence rate (28 cases per 100,000 male Arizonans) for late stage prostate cancer in Arizona between 2017 to 2021.
My story: Fred T of Glendale, Arizona

At 85 years old, I am not just a cancer survivor; I am a beacon of hope and an advocate for early detection of prostate and breast cancer. My journey began 25 years ago when, at the age of 60, I received a life-altering diagnosis of prostate cancer. My initial reaction was a mix of shock and fear, but I quickly turned my apprehension into action and gathered a cancer treatment team.
I immersed myself in learning about this cancer, understanding that knowledge would be my most powerful weapon. I chose seed implants, also known as brachytherapy, as my treatment method for prostate cancer. This decision, I believe, was crucial in my successful battle against the disease. Early detection was key; had my cancer been discovered at a later stage, I am certain my treatment options would have been limited and less effective.
Years later, in 2022, I faced another daunting challenge. During a routine self-check while showering, I discovered a lump on my right breast. This self-awareness, cultivated from my previous cancer experience, led me to seek immediate medical attention. A biopsy confirmed Stage 1A breast cancer. Despite the initial dread, I was relieved that my vigilance had paid off once again. My treatment involved five days of radiation therapy, and today, I proudly announce I am cancer-free.
What did you learn from your cancer journey?
I learned that early detection is crucial. It gives you more treatment options and a better chance of survival. I also realized the importance of being proactive about your health. You need to be your own advocate—ask questions, seek second opinions, and stay informed. Writing down questions and bringing someone to appointments to take notes can be incredibly helpful.
What would you like others to know about your journey?
I want people to know that taking responsibility for your health can save your life. Don’t wait for symptoms to appear; get regular screenings and perform self-checks. Early detection made all the difference for me. Additionally, don’t face it alone—bring a loved one to appointments for support and to help you remember the information provided by your doctors. Finally, stay hopeful and positive. It’s a challenging journey, but with the right mindset and support, you can overcome it.
Thanks to early detection, both cancers were treated successfully. Now, I am cancer-free and dedicated to helping others understand the importance of early detection and regular screenings.
Objective two: Increase the lung cancer screening rate among all high-risk Arizonans (per 2021 guidelines defined as those who are 50 to 80 years old and have a history of smoking for at least 20 pack years), from 1.3% to 6%.
Strategies
- Improve health care provider collaboration by partner with health care providers to ensure they recommend screenings during routine visits for all eligible patients, implementing training programs for health care professionals to enhance awareness and understanding of the importance of lung cancer screening.
- Focus on expanding community Partnerships by collaborating with community organizations, senior centers, and local business to spread and encourage participation in screening programs and leveraging existing networks to reach a broader audience.
- Implement media campaigns and increase public awareness by launching targeted media campaigns through TV, radio, and online platforms to reach the desired age group and emphasizing the importance of early detection and the benefits of lung cancer screening in reducing mortality.
Lung cancer cost data
$93,921 - The average cost of lung cancer related hospital discharges in Arizona 2022.
Approximately $186 million in total charges were spent on lung cancer related hospital discharges in Arizona in 2022.
Objective three: Increase colorectal cancer screening rates among Arizonans who are 45 years of age and older from 54% to 65%.
Strategies
- Advance health equity by expanding access to care and services through screening and patient navigation in an effort to promote the broad adoption of navigation reimbursement targeting rural and urban communities.
- Develop an evaluation tool to examine the intersectionality of evidence-based interventions and promising practices.
- Promote health systems and payer-based interventions such as patient reminders, provider reminders, provider assessment and feedback and actively engage in reducing structural barriers targeting rural and urban communities.
Colorectal cancer cost data
$115,099 - The average cost of colorectal cancer related hospital discharges in Arizona 2022.
Approximately $308 million in total charges were spent on colorectal cancer related hospital discharges in Arizona in 2022.
Colorectal cancer is the fifth most common cancer diagnosis and second leading cause of cancer death in Arizona. Between 2017 and 2021, approximately 58% of all colorectal cancer cases in Arizona were diagnosed late stage(Arizona Cancer Registry, 2017-2021).
Objective four: Decrease the percentage of late stage melanomas diagnosed in Arizona by 5%.
Strategies
- Establish a baseline to measure late stage melanoma diagnoses in Arizona.
- Update the Arizona Melanoma Profile and include additional demographic information to inform evidence-based interventions.
- The Melanoma Task Force will collaborate with community partners to increase educational outreach on early detection of melanoma in at-risk populations.
My story: Sharon M. of Phoenix, Arizona

When we're young and looking forward to starting our lives, cancer is rarely on our radar. As a young mother, I assumed fatigue was to be expected. But as my son aged into a toddler, my symptoms weren't improving. For me, that was exhaustion, to the point I could spend all weekend in bed.
As a freckle-faced redhead and former sunbather, I hadn't heeded the warnings to protect my skin when outdoors.Luckily for me, loved ones insisted I visit a doctor. Blood work, dietary changes, even vitamins provided little improvement. It was a visit to the dermatologist that solved the mystery. A mole on my lower back that I didn't know existed, turned out to be a malignant melanoma.
The good news is this visit saved my life. Melanoma is highly curable--when caught early. Mine was Stage 2. It had not advanced to my lymph nodes nor had it metastasized. An outpatient surgery enabled the mole to be removed, which included the skin around it to make sure cancerous cells were removed. That was 20 years ago and I've had two more malignant melanomas, but only Stage 1 because now I am aware of the importance of getting your skin checked every year or even more frequently. That means checking your scalp, between your toes behind your ears, and places that make me blush. And I've learned Melanoma doesn't only affect redheads like me, any skin color is susceptible to a potentially fatal skin cancer.
The older, wiser me, would suggest you keep your skin the color it was born in and when outdoors, wear your hat, some sunglasses, reapply sunscreen, and wear a lightweight long sleeve shirt even in the pool. Stay in the shade, especially during the middle of the day. And you can help the next generation reduce their chances of developing any form of skin cancer and living a long healthy life!
What did you learn from your cancer journey?
Get screened whether because of a concern you have--breast lump, rectal spotting, a mole that has changed, etc. and complete your annual screenings. You owe it to keep your appointment to yourself for both yourself and your family.
What would you like others to know?
Finding and identifying you have it is the first step toward getting better and treating it and living. There are wonderful organizations with great resources and support to help you with any form of cancer you may encounter.
Melanoma cost data
$51,124 - The average cost of melanoma related hospital discharges in Arizona 2022.
Approximately $4.1 million in total charges were spent on related melanoma related hospital discharges in Arizona in 2022.
Objective five: Increase the percentage of adolescent males and females ages 13 to 15 that are up to date with the human papillomavirus (HPV) vaccine series from 54.5% (females) and 60.9% (males) to 80.00% (males and females).
Strategies
- Utilize cross-sector collaborations within clinical and community-based settings that use evidence-based interventions to increase vaccination rates.
- Utilize health systems-based interventions (e.g., patient reminders, provider reminders, standing orders, provider assessment, and feedback, taking a presumptive approach to recommend the vaccine, bundling adolescent vaccines, motivational interviewing) and actively reduce structural barriers.
- Extend health care professionals’ (e.g., physicians, nurse practitioners, physician assistants, nurses, dentists, pharmacists, and school health providers) education to review and/or discuss the HPV vaccine status with age-appropriate patients at every clinical encounter.
- Build a culture of health across Arizona with a focus on under-resourced communities to improve health equity by educating community health workers about reducing the risk of HPV-related cancers through vaccination.
- Measure the progress of HPV vaccination coverage at the county level by examining ASIIS quarterly reviews on adolescents immunized against HPV.
Cervical cancer cost data
$60,338 - The average cost of cervical cancer related hospital discharges in Arizona 2022.
Approximately $11 million in total charges were spent on cervical cancer related hospital discharges in Arizona in 2022.
Objective six: Increase the breast cancer screening rate among all Arizonans who are 40 years of age and older from 68% to 75%.
Strategies
- Collaborate statewide on consistent, culturally tailored, public messaging for the current breast cancer screening evidence-based guidelines.
- Work with stakeholders to increase access to cancer-screening for low-income, uninsured, and other medically underserved populations identified through state and federal data sources.
- Educate primary care providers on the importance of a provider recommendation and adhering to nationally recognized, evidence-based breast cancer screening guidelines such as the United States Preventive Services Task Force (USPSTF), the National Comprehensive Cancer Network (NCCN), the American Cancer Society (ACS) and the American College of Radiology (ACR).
Breast cancer cost data
$71,331 - The average cost of breast cancer related hospital discharges in Arizona 2022.
Approximately $38 million in total charges were spent on breast cancer related hospital discharges in Arizona in 2022.
Female breast cancer is the most common cancer diagnosis and the fourth leading cause of cancer death in Arizona. Black/African American females have the highest age-adjusted incidence rate (152 cases per 100,000 female Arizonans) for late stage breast cancer in Arizona (Arizona Cancer Registry, 2017-2021).
My story: Ashley P of Glendale, Arizona

My story is a little more than just my own cancer journey. It actually started when my husband had thyroid cancer back in 2009. He was only 29 at diagnosis and had a full thyroidectomy three days after his 30th birthday. He not only had four cancer tumors in his thyroid, he had three in his lymph nodes and the tumors were two different types of thyroid cancer.
I was his caregiver throughout his treatment and, at times, struggled emotionally. It was hard to express because I was supposed to be the strong one so I had to turn to other people for support knowing he would never understand and that was ok. He is now (almost) 15 years NED.
Then in 2017 I was diagnosed with stage 2B triple negative breast cancer. At first I was angry, I was the healthy one in the family, I didn't have time for cancer. When I got over being angry, I embraced what was going to happen and knew that with positivity and strength I would get through and be fine. I went through six months of chemotherapy, where losing my hair was the worst part. After I finished chemo, I had a double mastectomy with reconstruction, then a followup surgery four months later.
It is a very different experience being the patient than the caregiver. People offer help and support to the patient, not even thinking about the caregiver. Since I had the unique experience of being the caregiver first, I tried to be a lot more patient with my husband and his emotions. Even asking those who were offering to help me to help him. After a few weeks, he sat down with me and said "I totally get it now, it is so hard to be the caregiver. You can't do much, you see the person hurting, you want to fix it or help but you can't." I honestly feel that being the caregiver was harder emotionally than being the cancer patient. I am now proud to say that I am (almost) seven years NED!
Being on both sides of the experience has taught me a lot. It's given me the unique perspective to help both the patient and their caregiver, or the new term that I prefer to use, co-survivor.
What did you learn from your cancer journey?
I learned so much! One of the main things that I learned was that positivity goes a long way than negativity or self pity. By staying positive gave me the strength to get through even the hardest days. While I did let myself have those bad days, I would remind myself who I was and what I was fighting for and change my mindset back to positive. I truly believe that I had a better outcome because of my mindset.
Another thing is that the co-survivor/caregiver also needs attention and help throughout the journey and that being the co-survivor can be a lot harder than being the cancer patient.
I also learned that you really have to be your own best advocate for health care and making sure that the insurance covers everything during and after treatment. A lot of insurance companies like to "play doctor" and tell you what they think you should have done instead of following what the doctor recommends. I learned how to really push back and stand up for myself and my family members when it came to making sure that they covered what was needed based on what the doctor said.
What do you want others to know?
First, I want everyone to know that each person's cancer journey is different. Everyone experiences things differently, feels things differently, and needs different things.
As for my journey, that is a little harder. I want everyone to know that just because someone's main treatment is over, it doesn't mean that they are done. Cancer can last for years, whether it is side effects, long-term medications, or just the follow up appointments. Specific side effects for me that still affect my daily life are chemo brain or brain fog which causes me to be forgetful and unable to think of words when I need them.
Treatment
Over the last twenty years, treatment has revolutionized the way we view cancer. With continuous improvement and innovation in the fields of research, technology, and delivery of care, we have seen a significant decline in the number and rate of cancer-related deaths as well as a rise in survival and improved quality of life.
By June of 2029
Objective one: Increase the number of cancer patients and survivors whose care team informs them about clinical trials from 22% (Cancer Experience Registry baseline, 2023) to 30%.
Strategies
- Integrate clinical trial education/opportunities into survivorship programming.
- Increasing clinical trial diversity by increasing awareness and education about clinical trials among patients and health care providers.
- Create a centralized resource to share clinical trials available in Arizona.
My story: Penny F of Prescott, Arizona

In 2015, I became a cancer survivor. I had a spot on my right forearm that just didn't look right. I asked my doctor about it on my next visit, and he wasn't too concerned but sent it out for a biopsy anyway. He called back about a week later and said two words that sent shivers down my spine: it's cancer.
It was an easy fix from there - the cancer was dug out of my arm and that was that. Until about a year ago. This time, I lost the top of my left ear. Again, it was all cut off.
This story actually started many years before this when I was growing up in California. Not only did we not wear sunblock...we would slather baby oil on ourselves to get a nice, deep tan! (Looking back now, all I can say is yikes!)
I now carry sunblock in my purse! It's not for me as I don't leave the house without sunblock but it is for anyone that I come across that needs it!
What did you learn from your cancer journey?
I learned how horrible it is to have your doctor say the words: you have cancer. I am also a "sunblock activist."
What would you like others to know?
It is preventable! We have some truly great products out there that can protect us. If I only knew then what I know now...Don't take a chance!
Objective two: Create and disseminate educational resources around kidney cancer incidence, mortality, and treatment.
Strategies
- Creation of educational resources (i.e. flyers, videos, presentation) that are culturally specific around Kidney Cancer.
- State Education platform - attend state-wide symposiums, conferences, advocacy and survivorship events to provide education around kidney cancer.
- Engage health care workers (primary care providers, urologists, community health workers, patient navigators) to help improve treatment journey - i.e. screening, treatment modalities, identifying signs and symptoms, Social Determinants of Health, and unique patient referral processes.
Kidney cancer cost data
$102,382 - The average cost of kidney cancer related hospital discharges in Arizona 2022.
Approximately $910 million in total charges were spent on kidney cancer related hospital discharges in Arizona in 2022.
Kidney cancer is the third most common cancer diagnosis and the fourth leading cause of cancer death for American Indians and Alaskan Natives in Arizona. American Indians and Alaskan Natives have the highest age-adjusted rates for new kidney cancer diagnoses (25 cases per 100,000 people) and deaths (seven deaths per 100,000 people), compared to all other races in Arizona (Arizona Cancer Registry, 2017-2021).
My story: James E of Fountain Hills, Arizona

I was the typical guy. It was definitely a guy thing, not going to the doctor yearly and focusing on going to work and home life. I started experiencing issues with urination and discomfort for quite some time, but I kept pushing it off.
Eventually, I went to the doctor to discuss my bladder issues. While I was at the office for a bladder scope procedure, with his back turned to me, my doctor casually mentioned, "It looks like you have cancer." I was in shock and disbelief. I wish the bedside manners were better. I went home and told my wife. We cried together, and once we collected ourselves, we started planning how to tackle this challenge.
Cancer wasn't new to me; several members of my family had been diagnosed with it, and I had always been the one offering support and advice. Now, I found myself on the receiving end. Faced with the situation, I realized that while I couldn't change the fact that I had cancer, I could choose how to handle it. I decided to maintain a positive attitude rather than succumbing to anger and frustration.
I opted for radiation therapy as my treatment. One of the most challenging aspects was ensuring I had a full bladder for each session. Through this experience, I discovered that many men suffer from prostate issues, but it's not commonly discussed. My journey highlighted the importance of talking about these health issues openly.
What did you learn from your cancer journey?
You can either be upset and go through it or up-beat and go through it, either way, you have to go through the cancer treatment. It is easy to be depressed and stressed. I chose a different path.
What would you like others to know about your journey?
From my cancer journey, I learned the critical importance of regular medical check-ups, even when you feel fine. Early detection can make a significant difference. I also discovered the power of a positive attitude. Choosing positivity helped me face each day with hope and strength.
My journey taught me the value of open communication with loved ones. My wife and I grew closer, learning to communicate more openly and listen better. This experience highlighted that cancer doesn't just affect the individual; it impacts the entire family. Their support and involvement are crucial for emotional and mental strength.
I want others to know that it's important to pay attention to your body and seek medical advice when something feels off. Don't ignore symptoms or delay doctor's visits. Prostate and bladder issues are common among men, and discussing them openly can lead to early detection and treatment, potentially saving lives.
Objective three: Decrease the length of time from diagnosis to treatment in lung cancer by 10%.
Strategies
- Encourage insurance companies to increase the network of specialists.
- Conduct a data analysis of the duration between lung cancer diagnosis and start of treatments by utilizing the National Cancer Database by the Commission of Cancer (CoC) of the American College of Surgeons.
- Identify gaps in access to medical oncology, radiation oncology or thoracic surgery by Federally Qualified Health Centers and Indian Health Service facilities.
Lung cancer cost data
$93,921 - The average cost of lung cancer related hospital discharges in Arizona 2022.
Approximately $186 million in total charges were spent on lung cancer related hospital discharges in Arizona in 2022.
Lung cancer is the second most common cancer diagnosis and the leading cause of cancer death in Arizona. More than a quarter of all cancer deaths (27.5%) can be attributed to tobacco (Arizona Cancer Registry, 2017-2021).
My story: Renae L of Phoenix, Arizona

When I was younger, my world turned upside down because both my mother and father were both diagnosed with cancer. First, it was my mom. She had breast cancer, but it was extra hard to treat because she also had lupus.
Not long after her diagnosis, my father was diagnosed with lung cancer. But instead of focusing on himself, he decided to take care of my mom. He said, "Two people can't be sick at the same time." So, he put all his energy into helping her, even though it meant he got sicker too.
It was a tough time for our family. We lost not just my parents but also other family members and friends to cancer. It felt like this scary cancer thing was always around us.
But I decided I didn't want to let cancer win. I knew I had to take care of myself to stay strong. I knew I needed to be physically, spiritually and mentally strong. I wanted to fight back against this thing that seemed to run in our family.
However, something special happened during that hard time. I talked a lot with my mom. She said she wished she had a better connection with her radiation therapist. So, I became her "honorary" therapist at home. I put up positive quotes all over the house and spent time just being with her, just being, laughing and listening.
My mother said something that has stayed in my heart and soul all of these years. She said I would make a great radiation therapist because when I was around, she felt like everything was going to be okay, even if just for a little while.
At that point, I decided to become a radiation therapist. I wanted to help others feel that same sense of hope and peace that I gave my mother.
Even though it is devastatingly painful to lose my parents and so many other family members and close friends, I didn't let it break me. Instead, I chose to be strong. I carry their love with me, and in all of their honor, I'll keep fighting against cancer with everything I've got.
What did you learn from your cancer journey?
I witnessed my father's sacrifice and unconditional love.
I experienced the importance of the healing power of empathy, support, and genuine human connection in navigating difficult circumstances.
I discovered a calling to help others facing similar struggles. It teaches the transformative power of finding purpose in pain, turning personal suffering into a force for good and channeling grief into positive action.
As a caregiver and a health care professional...taking care of people I know and love, I wanted the same thing they wanted...I didn't want them to have cancer; I didn't know why it happened to them; I wanted them to be cured; I wanted them to have peace and reassurance but all I can ever do is just be there and love like I know how and take care of them the best way I possibly could. Watching your loved ones and patients suffer hurts. Everyone that knows and loves a cancer patient/survivor is hurting. Our hurt is different from the patient, but it is still painful. Despite my deepest desires, I've come to terms with the fact that I cannot rewrite the fate of a cancer diagnosis; I will most certainly offer my unwavering support, my care, and my love.
My personal journey with cancer deeply influenced my decision to start a nonprofit organization. Watching my loved ones, family, and friends and patients that I treat, navigate the challenges of cancer treatment opened my eyes to the profound impact the disease has on individuals and their support networks (friends and families).
Ultimately, my experience with cancer ignited a passion within me to make a tangible difference in the lives of those affected by the disease. Through my nonprofit, I aspire to provide support that addresses the needs of patients, caregivers, and our communities.
Survivorship and quality of life
The term “cancer survivor” refers to someone living with, through, or beyond cancer from the moment of diagnosis through the end of life. This includes patients who are being treated for cancer, who are free of cancer, and who live with cancer as a chronic condition.
As with many chronic diseases, cancer survivors have unique medical, psychological and social needs that must be addressed. As this population and their caregivers continues to grow, ensuring that they have the proper care, support and resources in place is becoming increasingly important.
Overall cancer cost data
$110,426 - The average cost of cancer related hospital discharges in Arizona 2022.
Approximately $2.3 billion in total charges were spent on cancer related hospital discharges in Arizona in 2022.
By June of 2029
Objective one: Partner with at least 5 cancer survivorship support programs to disseminate National Cancer Survivor Standards of Care.
Strategies
- Conduct an Environmental Scan to identify stakeholders in Arizona and foster partnerships to determine the appropriate direction for dissemination.
- Identify updated National Cancer Survivor Standards of Care preferred method of dissemination in target population.
- Pilot dissemination of National Cancer Survivor Standards of Care with one partnering cancer survivorship support program to identify strengths and areas for opportunity in dissemination within additional support programs.
My story: Rachel S of Scottsdale, Arizona

Sadly, I was diagnosed while my husband and I were trying to get pregnant for the first time. It had been a year of trying so I visited my gynecologist to determine why this was proving so challenging for us. There were no symptoms that stood out glaringly to me. I believe it’s critical to raise ovarian cancer awareness so no other woman is blindsided with a diagnosis like I was.
What did you learn from your cancer journey?
Cancer can be scary, and it's something that no one can truly ever prepare for. I know this because I'm a two-time cancer survivor (breast and ovarian cancer). I want to ensure that every person impacted by these diseases knows they are supported, loved, and have an entire teal cancer community supporting them.
What do you want others to know?
One of my biggest missions in ovarian cancer is to educate others about the signs and symptoms of this terrible disease, as well as share my story about diagnosis and survivorship so that others are not blindsided like I was. Ovarian cancer research, awareness and funding needs to improve! I'm so sick of losing my friends, hearing of another newly diagnosed young person or supporting one of my sisters through yet another recurrence.
Objective two: Increase patient navigation events by 20% overall in underserved and rural communities.
Strategies
- Partner with employers within medically underserved communities to promote evidence based cancer survivorship programs and resources to their employees (i.e. lunch & learns)
- Using and regularly updating the ADHS cancer resource database, educate health care providers/patient navigators on available patient navigation events within their geographic areas using the ADHS Resources Registry by Patient Navigators at four (4) medical institutions.
- Promote twelve (12) local quality of life programs and or activities supporting the psychosocial needs of cancer survivors.
- Identify patient/survivor populations in underserved areas of Arizona needing access to cancer resources and events.
- Partner with hospitals/medical/state/tribal/local agencies that provide navigation/case management programs/activities that facilitate access to care and other issues, whether physical, or psychosocial, to cancer patients in rural/underserved communities.
My story: Lindsey B of Tucson, Arizona

My aunt Jan saved my life. It was my dear aunt Jan who prompted me to be proactive with my health and screening when she was diagnosed with BRCA1-positive ovarian cancer at the age of 65.
Despite learning of my BRCA1 status at the age of 33, and subsequently beginning regular imaging, I was diagnosed with Stage 2b, triple negative breast cancer (TNBC) at the age of 35. It was December 2020, the height of the global pandemic, when my surgical oncologist, who was monitoring me due to my high-risk status, informed me that in fact the lump I felt between scans was my biggest fear, breast cancer.
TNBC grows quickly, and I personally believe that had I not been aware of my genetic mutation or monitored, that my diagnosis would have been later stage and potentially terminal. The next 18 months were grueling. Undergoing cancer treatment during the midst of the pandemic was terrifying and extremely isolating. Six months of chemotherapy, multiple surgeries (including a double mastectomy and a bilateral salpingo oophorectomy), transfusions, and countless bags of IV fluids, blood draws, and doctors’ appointments, were all done solo, masked, and with the fear I wouldn’t reach my 40th birthday.
I am thankful to be here, healthy, happy, and just eight months away from reaching a milestone I was not sure I would have the chance to see.
What did you learn from your cancer journey?
- The importance of knowing your risk factors (dense breast, genetic mutations, age, etc.) and family history.
- Get to know YOUR normal.
I learned about “feel it on the first” from an incredible organization, The Breasties, that supports breast and gynecological previvors, survivors, thrivers, and caretakers.
What this means is doing a monthly breast self-exam at the same time every month; While this self-exam does not replace mammogram screening, becoming aware of your own breast changes with this quick self-check could save yours or a loved one’s life.
For me personally, despite completing breast imaging in June 2020, I developed a palpable lump in between scans. Doing a self-exam and discovering my lump in the shower, I believe is one of the reasons I am here today.
- Advocate.
You know your body better than anyone.
If something feels off, say something.
I am highly aware that as a nonprofit consultant who works to address social inequities, that significant health disparities exist in terms of access to care and clinical trials. Having met survivors of all ages, races, and socioeconomic backgrounds, I have heard too many stories of patients being dismissed. If you feel unheard, bring a trusted, loved one with you to your doctor’s appointment and/or consider switching physicians.
- Remember no one fights alone.
Should you find yourself diagnosed or caring for a loved one with breast cancer, we are fortunate to have many great local resources here in Southern Arizona and across the state. Seek support, ask for help, and find community.
Although more targeted resources are needed for the AYA cancer community.
Young adults and their loved ones will become more aware of the rising rates of cancer among adolescents and young adults (AYAs) and will be diligent about discussing cancer screening, prevention, and risk factors with their medical providers. Knowledge is power, and early diagnosis and treatment can be the difference between life and death.
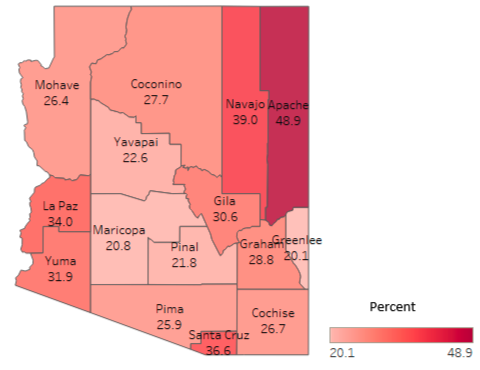
Figure 3.1: Social Vulnerability Index Score Ranked 0 (least vulnerable) 1 (most vulnerable) by County-Arizona, Social Vulnerability Index Data 2021
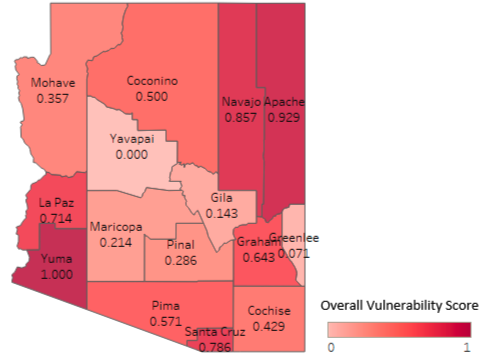
What is social vulnerability?
Every community must prepare for and respond to hazardous events, whether a natural disaster like a tornado or a disease outbreak, or an anthropogenic event such as a harmful chemical spill.
The degree to which a community exhibits certain social conditions, including high poverty, low percentage of vehicle access, or crowded households, may affect that community’s ability to prevent human suffering and financial loss in the event of disaster. These factors describe a community’s social vulnerability.
What is the Centers for Disease Control/Agency for Toxic Substances and Disease Registry (ATSDR) Social Vulnerability Index?
ATSDR’s Geospatial Research, Analysis, and Services Program (GRASP) created the Centers for Disease Control and Prevention and Agency for Toxic Substances and Disease Registry Social Vulnerability Index (CDC/ATSDR SVI or simply SVI) to help public health officials and emergency response planners identify and map the communities that will most likely need support before, during, and after a hazardous event.
SVI indicates the relative vulnerability of every U.S. Census tract. Census tracts are subdivisions of counties for which the Census collects statistical data. SVI ranks the tracts on 16 social factors, including unemployment, racial and ethnic minority status, and disability, and further groups them into four related themes. Thus, each tract receives a ranking for each Census variable and for each of the four themes as well as an overall ranking
Why SVI?
SVI data identifies communities that are more vulnerable due to socioeconomic factors such as income, education level, housing status, and access to healthcare. By incorporating this data into a cancer plan, resources can be allocated more effectively to these underserved, and disproportionately impacted populations. SVI data also provides evidence for advocacy efforts aimed at policy level change. It can highlight the need for policies that address the root causes of health disparities, such as poverty and lack of access to healthcare. Since different communities have different cultural beliefs and varying levels of health literacy, understanding SVI also helps tailor outreach and education efforts.
Including SVI data in the Plan enhances its ability to address disparities, tailor interventions to specific community needs, and promote equitable access to cancer care across all populations within the state.
Objective three: Decrease the percent of survivors of cancer reporting food insecurity to ensure access to high-quality nutritious food to contribute to overall health.
Strategies
- Identify hospitals and health care settings in Arizona that screen patients for food insecurity and offer programs to connect patients to resources for health food access.
- Identify potential Partner Farms in Arizona to supply/stock food pantries specifically to connect cancer patients to healthy, whole-food options.
- Increase assessment of food insecurity and referral to emergency food systems (e.g., Supplemental Nutrition Assistance Program, food banks, financial assistance) in oncology practices/cancer centers.
Figure 3.2: Estimated percentage of Arizona households who receive food stamps/SNAP benefits by county-Arizona Social Vulnerability Index 2021/American Community Survey 2017-2021
Objective four: Increase participation in the Arizona Cancer Experience Registry (CER) from 70 to 350 participants by June of 2029.
Strategies
- Create partnerships with other organizations that serve underrepresented populations to disseminate the survey.
- Increase accessibility for Spanish speakers so Latino communities can complete the survey.
- Increase participation from those struggling with financial toxicity.
- Create and disseminate CER findings in an annual report to coalition and partners.
My story: Julie D of Phoenix, Arizona

Two years ago, at age 47, I was diagnosed with breast cancer. I never thought it would happen to me, because I was young, healthy, and I felt fine. But a routine mammogram led to my world turning upside down. Luckily, I had the support of my family and friends to get me through it.
I had surgery, chemotherapy, and radiation. I lost all my hair. That part was very difficult. I had to stop working to focus on recovery, which added financial stress to me and my family. And I worried about how my daughter was going to feel seeing her mom go through this terrible disease. She was only 12 years old, and had her own journey as part of this.
Cancer affects the whole family, not just the patient. But thankfully, I responded well to treatment and am now on hormone therapy for five years. As a survivor, I discovered the services of Cancer Support Community Arizona, a nonprofit that provides free social and emotional support to people impacted by cancer, where I now work.
I am glad I get to help others navigate their cancer journey, and find community so they feel less alone, more in control, and have hope.
What did you learn from your cancer journey?
I learned how important it is to ask for help. No one should face cancer alone, and there are so many great free resources available in the community to help people going through a cancer journey. It takes courage to ask for help.
What would you like others to know?
I want others to realize how important it is to go for regular physicals and cancer screening tests. I was lucky, my cancer was caught in stage one. That means my treatment wasn't as hard as it could have been. Don't get me wrong, chemo was hard, but I always felt like I was going to get through it because it was caught early.
Policy
About half of cancers are preventable through lifestyle, diet, exercise and environmental changes. However, people are also influenced by often powerful forces. Many of the changes that would lead to better cancer outcomes are best driven by proven, evidence-based policies. Included in this section of the Arizona Cancer Plan are policy objectives that could help our state reduce the cancer burden.
By June of 2029
Objective one: Secure legislative support to expand health care access through patient navigation for Arizona cancer patients.
Strategies
- Educate the executive and legislative branches of the Arizona government on patient navigation best practices.
- Establish a Cancer Caucus within the Arizona Legislature to advocate for patient navigation at the state level.
- Secure funding to support patient navigation resources in rural and underserved communities.
Figure 3.3: Estimated percentage of Arizona households who are uninsured by county-Arizona Social Vulnerability Index 2021/American Community Survey 2017-2021.
My story: Anna V of Phoenix, Arizona

I had never heard of ovarian cancer. Breast cancer, yes; lung cancer, yes; pancreatic cancer, yes. Prostate cancer is well documented on my dad’s side of the family, but OVARIAN cancer? I'd never heard of it, never knew anyone who had it.
During a road trip to California, I talked to my husband about the bundle of ailments I was experiencing. We both agreed that I should contact someone when we returned to Phoenix. Easier said than done: my gynecologist had retired a few years earlier, and I wasn’t excited about finding a new one.
The doctor sent me for a transvaginal ultrasound and two hours later, I was told there were vascular masses on my ovaries, and all signs pointed to cancer. A CT scan the next day staged my cancer at 3C. I had a hysterectomy and debulking surgery on May 20, exactly two weeks after my first appointment. I started chemotherapy with Carboplatin and Taxol three weeks later of six infusions three weeks apart.
In October 2016, I felt the pain in my lower left side. It persisted, so I moved my routine CT scan up. The scan on Nov. 17 showed a mass near my left descending colon. The cancer had returned. The second debulking resulted in removing half of my left descending colon followed by six sessions with the Doxorubicin and Carboplatin. Then I started a PARP inhibitor for maintenance and have been NED (No Evidence of Disease) for three and a half years.
What did you learn from your cancer journey?
My chronic anxiety and its chorus of "What Ifs" created a vicious, paralyzing cycle, holding me back from things I wanted to do. I was determined to break the cycle. I faced the anxiety by banishing the "What Ifs" and embracing the "Why Not" attitude.
What would you like others to know?
I must add that there was a silver lining to the dark cloud of recurrence: the bowel resection cured my Irritable Bowel Syndrome! The theory is that the cancer attacked the weakest part of my body, which happily turned out to be the irritable part of my bowel.
While I try to find the silver lining in every dark cloud, I’m also a realist: I know I’ll be checking my rearview mirror for ovarian cancer for the rest of my life. Therefore, I continue to move forward in promoting cancer awareness, advocating for new therapies, and one day, a cure.
I took my fear and turned it into a brave, confident, empowering force to be reckoned with. I am committed to educating all about the early signs of this cancer and sharing my experiences in the hope it helps other women to know about ovarian cancer.
Objective two: Increase state-funded cancer screening programs for cancer types with medical consensus on screening recommendations
Strategies
- Educate and raise awareness on the importance of cancer screening with legislators.
- Secure funding of mobile units for health equity cancer screening to census tract locations and geographic regions with low screening rates and social vulnerability indexes.
- Identify gaps in access to medical oncology, radiation oncology or thoracic surgery by gathering feedback from community members and performing at least one community needs assessment.
- Explore the process for state funding (license plate) to be allocated to a new cancer awareness/screening program.
Figure 3.4: Estimated percentage of Arizona households who are below 150% poverty estimate by county-Arizona Social Vulnerability Index 2021/American Community Survey 2017 to 2021
Objective three: The percentage of cancer cases reported on time according to regulation will increase from 27% to 75%.
Strategies
- Develop and disseminate materials on the importance of cancer reporting signed by coalition stakeholders with the goal of informing hospital administrators.
- Develop and implement a quality improvement process that incorporates sharing of hospital cancer reporting information with the goal of encouraging more timely reporting.
- Increase electronic cancer reporting from providers/clinics.
Objective four: Reestablish Arizona as a leader in Tobacco Control policy by garnering legislative support to sponsor at least (1) bill that would implement evidence based tobacco control policies.
Strategies
- Leverage the Students Taking a New Direction (STAND) coalitions for educational outreach to elected officials regarding tobacco control best practices.
- Establish a formal tobacco control coalition to bring community stakeholders, state agencies, and other interested parties together on a regular basis to discuss trends and goals for future action.
- Establish tobacco control partnerships with tribal entities to address tribal specific tobacco challenges.
My story: Miguel R of Laveen, Arizona

I’ve had several family members pass away from cancer. It’s part of why I’ve volunteered with the American Cancer Society Cancer Action Network (ACS CAN). Advocate for more funding for cancer research. My paternal grandfather died of lung cancer which was a result of his smoking. Supporting responsible and sensible tobacco legislation is something that is important to me.
What did you learn from your cancer journey?
That we should use our voices to advocate for others. To lobby our representatives to support cancer patients and their families by supporting legislation that will fund cancer research, provide funding for cancer screening and legislation that makes navigating insurance easier for patients and their families.
Childhood cancer
Thankfully, improvements in detection and care have led to significant increases in the number of pediatric cancer patients who survive their diagnosis. Furthermore, mortality rates of childhood cancer have declined over the past four decades thanks to improvements in treatment and high rates of participation in clinical trials. Early diagnosis of childhood cancer can be challenging because symptoms are similar to those of more common childhood illnesses.
By June of 2029
Objective one: Host at least three opportunities for health care providers to learn more about diagnosis and management of pediatric cancer patients and survivors of childhood cancer diagnosis.
Strategies
- Develop a target provider group and content for the three events with a greater emphasis on research,clinical trials, and effective treatment options.
- Host two in-person, and one virtual Grand Round as an on-going learning opportunity(or Continuing Education.)
- Facilitate at least one conference for pediatric cancer advocates to collaborate.
My story: Beverley T of Tucson, Arizona
My son William was diagnosed with a brain tumor (anaplastic ependymoma) when he was four years old. I was seven months pregnant when he was diagnosed and I knew there was something wrong with William but his pediatrician insisted he had “sympathetic vomiting” in response to my vomiting due to my pregnancy. I was diagnosed as a “neurotic mother” such that when I arrived in the middle of the night to ER with my ailing son, his pediatrician insisted on sending us home – I refused to leave the ER and at 7:00 a.m. when the morning staff arrived my son was given a CAT scan which detected the grapefruit sized mass near his temporal lobe.
In Tucson he underwent two neurosurgical procedures and his neurosurgeon determined his tumor was inoperable. Our family took health seriously and we were careful about what we ate and drank and what our children were exposed to so this diagnosis was beyond challenging.
Our second son was born the same day his older brother William was discharged from hospital after being given his first chemotherapy and a broviac catheter inserted into his chest to access the superior vena cava vein for future procedures and IV access. After chemotherapy proved unsuccessful we reluctantly agreed to 5800 rads of cranial radiation to his tumor. This also proved unsuccessful.
We communicated with a lot of people around the country and we eventually found a pediatric neurosurgeon at New York University Medical Center – Fred Epstein MD, who was a pioneer in complex pediatric neurosurgical procedures.
We decided to risk it all and went to New York City. My neurosurgeon here in Tucson told us not to bother coming back to him if we went out of town for services. The head of radiation oncology at Banner UMC yelled at me saying I was taking my child’s life into my own hands and that William might die in NYC – I figured dead was dead whether in NYC or Tucson, we figured the odds were better in NYC.
Although my son's tumor was considered inoperable in Tucson after chemotherapy and radiation, we found a pediatric neurosurgeon in New York who was able to remove the whole tumor. This required a cross country life saving trip. No one in Tucson suggested we go to Barrow or Phoenix Children’s hospital.
The tumor recurred again after five years followed by another successful resection then a third occurrence at age 11 eluded treatment of stereotactic radiation and he passed away after a seven-year battle with a brain tumor.
This was an unimaginable trauma to our whole family and his siblings will spend a lifetime trying to overcome the pain from the loss of their brother and the prior medical dramas surrounding treatment and relapse.
As parents, it is the most excruciating experience to endure treatment and recurrence of cancer then to have to bury one's child. I would like to see childhood cancer treatment modalities improve. A child diagnosed with a brain tumor should be provided a comprehensive neuro-oncology team to address everything from surgery to best treatment options, including proton therapy radiation.
What did you learn from your cancer journey?
Advocacy for one's child is key to optimal treatment and outcome.
What would you like others to know?
Take the bull by the horns - join others in the struggle - provide resources and services for siblings. (Camp Sunrise Sidekicks). Treat all children equitably in the family. Be kind to your other parents - if the medical community doesn't have ideal treatment for your child, as parents you are on a bumpy road. Drove carefully. Cancer sucks! Treatment sucks also! We need more funding to find better treatment. "...Ologists" aren't always right. It's ok to travel out of state. Insurance costs can be appealed.
Objective two: Develop five cancer literary resources for parents, providers, and community partners with epidemiological data about the top cancer diagnosis for children in Arizona.
Strategies
- Partner with the Arizona Department of Health Services Office of Children and Youth with Special Health Care Needs to engage partners in performing a landscape assessment of local needs and resources to help inform the crafting of a profile for communities with a high burden of child cancers and need for support.
- Develop at least three fact sheets geared toward informing professionals who engage school-age children (i.e. general practice providers, emergency providers, school nurses, physical education instructors, and/or Community Health Workers).
- Develop at least two pamphlets with real Arizona stories for difficult to diagnose childhood cancers.
- Develop a communication plan for which to distribute fact sheets.
- Continue to engage and support local partners in promoting the awareness of childhood cancer and survivorship support through strategic distribution of the newly developed literary resources.
My story: Sergio, P of Phoenix, Arizona

The summer before my freshman year of high school, as I was getting ready for little league, I was diagnosed with osteosarcoma in my left knee. That summer I would not be preparing to take the field as a capable, young, healthy high school athlete. Instead I would learn to ask for help for the most basic things - no easy transition, I can assure you. I never made it back to the field that summer but with some help from my community and a few special accommodations, I was able to play baseball again!
The biggest lesson learned from my battle with cancer was the value of empathy. With cancer there is a lot of stress and luckily I had lots of hands on deck to support me through treatment and even through today. No one person can defeat cancer. My family and medical team got me through treatment. My community's empathy and support brought me back in from the cold and lonely isolation someone might feel when they are differently abled.
"What does not end you, makes you stronger!" After surviving cancer in high school, I remember hearing this a lot. While I am sure folks meant this to be a positive statement, I knew they were wrong. My body had battled cancer and every cancer survivor is a wounded warrior.
What did you learn from your cancer journey?
Cancer happens! It is not fair and there is no denying that. Compassion from others helps soften the blows from day to day and you know - it is something we can all offer to each other for free, even if cancer is not present.
What do you want others to know?
Early detection and prevention can be key in surviving cancer and provide peace of mind, especially if you already have survived a cancer before.
Objective three: Support and promote community engagement for survivors of childhood cancers with development of best practices.
Strategies
- Partner with community based organizations in the childhood cancer community to promote resources on the ADHS webpage by April 30, 2026
- Develop best practices for a mentorship program to be used by oncology clinics to support patients in the long term through survivorship by June 30, 2026.
- Develop and distribution/promotion plan for the mentorship best practices by June 30, 2026.
Resources
Arizona Cancer Programs
Arizona Comprehensive Cancer Control Program (AzCCCP)
The Centers for Disease Control and Prevention (CDC) defines Comprehensive Cancer Control as “a collaborative process through which a community pools resources to reduce the burden of cancer that results in risk reduction, early detection, better treatment, and enhanced survivorship.” The program facilitates the coalition and moves the work of the state plan forward through its programming. The program is funded by the CDC.
Well Woman HealthCheck Program (WWHP)
The Well Woman HealthCheck Program (WWHP) was established in 1993 as part of the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) administered by the Centers for Disease Control and Prevention.
In Arizona, the WWHP is part of the Bureau of Health Systems Development at the Arizona Department of Health Services. The program helps low-income, uninsured, and underinsured women gain access to breast and cervical cancer screening and diagnostic services, including: clinical breast exams, mammograms, pap tests, and pelvic exams. Diagnostic testing includes tests like ultrasounds, biopsies, and other tests that are also available if screening results are abnormal. Referrals are made for treatment as necessary.
Additionally, the Well Woman HealthCheck Program helps verify the eligibility and facilitate the enrollment of uninsured women in Arizona diagnosed with breast or cervical cancer or precancerous cervical lesions into the Breast and Cervical Cancer Treatment Program (BCCTP) provided by the Arizona Health Care Cost Containment System (AHCCCS). The WWHP receives funding from the CDC, state match, and breast cancer license plate program.
The Arizona Cancer Registry (ACR)
The ACR is a population-based surveillance system that collects, manages and analyzes information on the incidence, survival and mortality of persons having been diagnosed with cancer.
The purpose of the ACR is to monitor cancer incidence patterns, promote and assist hospital cancer registries, improve and maintain standards for the quality of information gathered relating to the detection, diagnosis, and treatment of persons diagnosed with cancer, identify population subgroups at high risk for cancer that need intervention programs or epidemiologic research, detection and prevention, and perform epidemiologic studies, and to provide biostatistic and epidemiologic information to the medical community. The ACR is funded by the CDC and state-matched funds.
Glossary of terms
Age-adjusted rates
Age adjustment is a process used to compare incidence and mortality rates over time or among geographic areas or populations that have different age distributions. Because most disease rates increase with age, age adjustment eliminates the confounding effect of age when comparing rates. Cancer incidence and mortality is usually expressed in the number of new cases or deaths per 100,000 persons in a population.
Age-specific rates
The rate of incidence or mortality of a specific age group, calculated per 100,000 people.
Alternative therapy
Alternative therapy refers to treatments that can be used in place of the standard cancer treatments. The standard cancer treatments are backed by science and are accepted by medical experts as a proper treatment for cancer.Alternative therapy is not the standard of care.
Best practices
A practice supported by a rigorous process of peer review and evaluation indicating effectiveness in improving health outcomes, generally demonstrated through systematic reviews.
Built environment
The built environment is defined as the human-made features of our communities. The way we design and build our communities can affect our physical and mental health; in turn designing and building healthy communities can improve the quality of life for all people.
Cancer burden
An estimate of the financial, emotional, or social impact that cancer creates within the population. Different racial, ethnic, geographic, and age groups in the United States do not share the burden of disease equally.
Cancer survivor
An individual is considered a cancer survivor from the time of diagnosis, through the balance of his or her life. Family members, friends, and caregivers are also impacted by the survivorship experience and are therefore included in this definition.
Caregiver
Any person who helps or supports a person who has been diagnosed with cancer.
Chronic cancer
Cancer that can not be cured but can be controlled with treatment for months or even years. Chronic cancer never completely goes away.
Complementary therapy
Refers to treatments that can be used in addition to the standard cancer treatments. This is called integrative medicine when it has been discussed with and approved by your health care team.
Community health worker/Community health representative/Promotora
Trained public health workers that serve as a bridge between communities, health care systems and state health departments. They are instrumental in promoting community health, bridging gaps in health care access, advocating for health equity, improving care coordination, and fostering trust between communities and health care systems.
Co-survivor
Sometimes used to describe a person who has cared for a person with cancer (e.g. family, friend, supporter).
Distant stage
Cancer that has spread from the primary site to distant organs or distant lymph nodes.
Early stage
Early stage combines in situ and local stage using the SEER Summary Stage guidelines.
Evidence Based Intervention (EBI)
Evidence-based practices are approaches to prevention or treatment that are validated by some form of documented scientific evidence. This includes findings established through controlled clinical studies, but other methods of establishing evidence are valid as well.
Federally Qualified Health Centers (FQHCs)
Organizations receiving grants under Section 330 of the Public Health Service (PHS) Act. FQHCs qualify for enhanced reimbursement from Medicare and Medicaid, as well as other benefits. FQHCs must serve an underserved area or population, offer a sliding fee scale, provide comprehensive services, have an ongoing quality assurance program, and have a governing board of directors.
Health care team
The health care team is the group of professionals who work together to care for and treat a cancer patient. They are from different health care areas who work together to provide care to patients. The team members bring their knowledge, skills, and expertise to address various aspects of patient care, aiming to improve health outcomes and patient satisfaction.
Health equity
Health equity is a public health concept that is rooted in equality and inclusion. As defined by the American Public Health Association (APHA), health equity is achieved when every person has the opportunity to attain his or her full health potential and no one is disadvantaged because of social determinants of health (SDOH) such as income, environment, educational attainment or access to health care.
Health promotion
Health promotion is the process of enabling people to increase control over, and to improve, their health. It moves beyond a focus on individual behavior towards a wide range of social and environmental interventions.
Health risk factors
A risk factor is any attribute, characteristic or exposure of an individual that increases the likelihood of developing a disease or injury.
Integrative medicine
Integrative medicine is complementary medicine that has been discussed with and approved by your health care team.
Integrative/Complementary care
To try and improve cancer outcomes, integrative/complementary care focuses on health aspects such as nutrition, exercise, stress management and sleep habits. They are affordable practices that have a solid safety record and are evidence-based. Complementary/integrative care adds to and supports standard cancer treatment. These therapies may include but are not limited to: acupuncture, massage, tai chi, music therapy, nutrition counseling, exercise, mind-body techniques such as meditation, yoga, imagery, relaxation, and breathing techniques.
Cancer (In Situ)
Early cancer that is present only in the layer of cells in which it began. There is no penetration of the basement membrane of the tissue.
Incidence
The number of newly diagnosed cases of cancer during a specific time period. Invasive Cancer Cancer that has spread beyond the layer of tissue in which it developed and is growing into surrounding, healthy tissues -- generally, the stage is either "localized," "regional," or "distant."
Late-stage
A term used to describe cancer that is far along in its growth, and has spread to the lymph nodes or other places in the body. Late-stage combines regional and distant stage using the SEER Summary Stage guidelines.
Localized stage
Cancer that is limited to the organ in which it began, without evidence of spread.
Metastasis
The spread of cancer cells from the place where they first formed to another part of the body. In metastasis, cancer cells break away from where they started, travel through the body and form a new tumor in a new area of the body, but it is still the original cancer. For example, if breast cancer spreads to the lung, the cancer cells in the lung are breast cancer, not lung cancer.
Mortality
The number of deaths from cancer during a specific time period.
Palliative care
Specialized medical care for people with serious illnesses. It is focused on providing patients with relief from the symptoms, pain, and stress of a serious illness—whatever the diagnosis. The goal is to improve quality of life for both the patient and the family Patient Navigator Patient navigators—a diverse group of lay people and health care professionals who assist patients at all stages of cancer care, from screening and diagnosis to treatment and survivorship.
Patient navigator/Patient advocates
Patient navigators/Patient advocates work with cancer patients and their families to help them overcome obstacles in the health care system or to find resources. They may help with: disease research, insurance problems, finding doctors, understanding treatment and care options, going to doctor visits with them, serving on their health care team, working with family members and caregivers, mobilizing resources, managing medical paperwork, and many other areas of support .
Peer support
Peer support is when people use their own experiences to help each other. They provide information, lessons learned, a listening ear, resources, and hope to other survivors or caregivers. Peer support may be provided by trained peers such as a patient navigator or community health worker. Peer support may also consist of interaction with cancer survivors or caregivers.
Policy, Systems, and Environmental (PSE) change
PSE approaches can make healthy living easier and provide sustainable cancer prevention and control improvements where people live, work, play, and learn. We can make communities healthier by supporting changes in:
- Policies to protect communities from harmful agents or elements (such as indoor tanning policies to limit exposure to ultraviolet rays or smoke-free policies to limit exposure to secondhand smoke).
- Systems to increase the use of client reminders to get people screened for cancer, or to increase access to healthy food choices in schools and workplaces.
- Environments to encourage communities to be active (such as pedestrian-and bike-friendly streets).
Prevalence
The number of people alive on a certain date who have been diagnosed with cancer at any time in their lives. This is different from incidence in that it considers both newly diagnosed and previously diagnosed people.
Quality of life
The overall enjoyment of life. Many clinical trials assess the effects of cancer and its treatment on the quality of life. These studies measure aspects of an individual’s sense of well-being and ability to carry out various activities.
Recurrence
Cancer that has come back, usually after a period of time when the cancer could not be detected. The cancer may come back to the same place in the body as the original tumor (local recurrence) or to another place in the body (distance/metastatic recurrence).
Regional stage
Cancer that has spread beyond the original (primary) site to nearby lymph nodes or organs and tissues.
Remission/No evidence of disease
This means that no cancer can be found in the body right now. This may be based on scans, bloodwork, or some other kind of test, such as a breast biopsy or a bone marrow biopsy.
Screening (Cancer)
Cancer screening is looking for cancer before a person has any symptoms. Screening tests can help find cancer at an early stage, before symptoms appear. When abnormal tissue or cancer is found early, it may be easier to treat or cure. By the time symptoms appear, the cancer may have grown and spread. This can make the cancer harder to treat or cure.
Social Determinants of Health (SDOH)
The social determinants of health (SDOH) are the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies and political systems.
Stable disease
Cancer that is not getting worse or better.
Stage
Stage provides a measure of disease progression, detailing the degree to which the cancer has advanced.
Survivorship care plan/Follow-up care plan
A detailed plan (sometimes called a survivorship care plan) given to a patient that contains a summary of the patient’s treatment, along with recommendations for follow-up care. In cancer, the plan is based on the type of cancer and the treatment the patient received. A follow-up care plan may include: schedules for future physical exams and medical tests. Additionally, it may include referrals to specialists and recommendations for a healthy lifestyle. You can share this plan with your noncancer health care providers as needed.
Treatment plan
A detailed plan with information about a patient’s disease, the goal of treatment, the treatment options for the disease and possible side effects, and how long treatment is expected to take. The treatment plan is separate from the follow-up care plan/survivorship care plan. Ideally everyone has both plans.
Evaluation process
An evaluation team from LeCroy & Milligan Associates, Inc. was engaged to monitor process and outcome evaluation measures for the activities within the Coalition. A comprehensive evaluation plan was developed to measure the 20 objectives determined by the AzCC Work Groups. Continuous evaluation of the work and process within the Action Teams, Steering Committee, Core Team, and the AzCC as a whole guides the coordination of work being conducted throughout Arizona and ensures activities are focused, effective, and aligned with statewide objectives.
The evaluation team provides support to the Steering Committee and Work Groups by assisting with the planning and facilitation of Action Team meetings, identifying the activities of the workgroups that align with their work groups’ objectives and goals, providing ad-hoc professional development and data analysis technical assistance for work groups’ activities and reporting on quarterly progress within work groups’ action plans. In addition, the evaluation team provides expertise and coordination among collaboration opportunities between the Core Team and all components of the Program. Meetings are assessed based on their level of effectiveness, collaboration, and quality of leadership. For additional information about the evaluation team and their processes, please visit LeCroy & Milligan Associates’ website.
Acknowledgments
Arizona Department of Health Services Division of Prevention
- Cassandra Webb, MPH, Program Manager, Comprehensive Cancer Control
- Tenneh Turner-Warren, MS, Office Chief, Chronic Disease & Population Health
- Polar S. Akoi, RDH, MPH, Cancer Program Administrator
- Lesleigh Zerby Higgins, MPH, Well Women Health Check Program Manager
- Katherine Steele-Watson, Program Manager, WISEWOMAN Program
- Anna M. Alonzo, Arizona Cancer Coalition Program Support
- Sheila Sjolander, MSW, Deputy Director of Public Health Services, ADHS
- Celia Nabor, MPA, Assistant Director for Prevention Services at the Arizona Department of Health Services, ADHS
- Teresa Aseret-Manygoats, MPA, Bureau Chief, Bureau of Chronic Disease and Health Promotion and the State Chronic Disease Director, ADHS
Community Leadership Team
- Brian Hummell, Arizona Director of Government Relations, American Cancer Society Cancer Action Network
- Abhinav Chandra, MD, Executive Medical Director of Specialty Care Services, Yuma Regional Medical Center
- Jaime Aiken, Regional Manager, National Ovarian Cancer Coalition
- Renae Linden, RTT, Chief Radiation Therapist/Founder, Cancer Matters
- Sergio Perez, MPA, Strategic Initiatives Lead, Policy & Intergovernmental Affairs, ADHS
- Georgia Armenta Yee, BSW, Health Registries Systems Manager, ADHS
- Dana Doyle, MPH, Epidemiologist, Arizona Cancer Registry, ADHS
- Amanda Swanson, MPH, Epidemiologist II, Bureau of Assessment and Evaluation, ADHS
Evaluation Team
- Michele Schmidt, MPA, Senior Evaluation Associate, Lecroy & Milligan Associates, Inc.
- Yvonne Bueno, DrPH, MPH, Senior Evaluation Associate, Lecroy & Milligan Associates, Inc.
Review Team
- Dr. Monica Yellowhair, University of Arizona Cancer Center, Office of Community Outreach and Engagement
- Ralph Ranger, PhD Just Evaluation Services
- Chavon Woods, MPA Office of Health Equity, ADHS
- Rebekah Kamer, Bureau of Assessment and Evaluation, ADHS
Communications and Web Development Teams
- Jesse Lewis, Communications Director, ADHS
- Megan Thomas, Content Manager, ADHS
- Omar Villalobos Castro, Web Developer, ADHS
Contributing partners
We thank the following national, state and community partners and organizations for generously giving their time and energy to the Arizona Cancer Coalition.
|
American Childhood Cancer Organization American Cancer Society Cancer Action Network American Lung Association Arizona Biomedical Research Center, ADHS Arizona Cancer Foundation for Children Arizona Center for Tobacco Cessation – ASHLine Arizona State University Arizona Prostate Cancer Coalition Bag IT! Banner Medical Anderson Cancer Center Cancer Matters Cancer Support Community Arizona Candlelighters Childhood Cancer Foundation of Southern Arizona Chiricahua Community Health Centers, Inc. City of Hope Phoenix Colorectal Cancer Alliance Exact Sciences Hopi Cancer Support and Tobacco Program Hopi Women’s Health Program Indian Health Services Johnson & Johnson, Inc. Kingman Regional Medical Center |
Mayo Clinic Arizona/Comprehensive Cancer Center Merck & Co., Inc. Mariposa Community Health Center National Association of Chronic Disease Directors National Ovarian Cancer Coalition Northern Arizona University Pfizer, Inc. National LGBT Cancer Network National Native Network Native Americans for Community Action North Country HealthCare North American Quitline Consortium Phoenix Children’s Pima County Health Department Pinal County Health Department Southwest Navajo Tobacco Education Prevention Program Susan G. Komen Foundation The Translational Genomics Research Institute University of Arizona, Helpers Program University of Arizona, Tobacco Cessation Training Institute University of Arizona Cancer Center University of Colorado, Anschutz Medical Campus Wesley Community and Health Center Yuma Regional Medical Center |
The 2024-2029 AzCCP was made possible by Cooperative Agreement Number NU58DP007089-01-00, funded by the Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or the Department of Health and Human Services.
Suggested Citation: Arizona Department of Health Services. (2024). Arizona Cancer Control Plan, 2024-2029. Phoenix, AZ: Arizona Department of Health Services, Bureau of Chronic Disease and Health Promotion, Office of Cancer Prevention and Control.
For more information about this plan, please visit our Arizona Cancer Coalition page.